Alternative knee operations
Contents:
- Arthroscopic “shaving” and other procedures
- Transplantation of tissues and cells
- Osteotomy
- Arthrodesis
Arthroscopic – key hole- operations
Meniscus resection
In patients with moderate osteoarthritis of the knee joint, the patient may complain more of stiffness, catching, and other difficulties to move the knee joint than the pain itself. These complaints may be caused by rupture of the degenerated meniscus, by a piece of avulsed joint cartilage or by roughly joint surfaces that hinder free motion in the knee joint.
The surgeon can examine the knee with an arthroscope and remove the hindrances.
The surgeon may remove the torn meniscus, remove the large pieces of avulsed joint cartilage that float in the joint space, shave the rough joint cartilage surfaces to a clean, smooth level. This is called arthroscopic debridement.
The value of this procedure for treatment of knees damaged with osteoarthritis is still discussed. Large statistics show that 70 % of all patients >70 years of age were still satisfied with their knee three years following arthroscopic debridement. (Wai 2002).
The advantages:
- It is a small procedure with few risks, that is suitable for older patients.
The disadvantages:
- The procedure offers seldom a lasting cure for ostoarthritic complains.
- In older patients this procedure may unnecessarily postpone a total knee replacement which offers a definitive treatment of osteoarthritic knees.
Transplantation of knee joint tissues and cells
Transplantation of patient’s own living cartilage cells.
This operation method is not applicable for knee joints damaged with osteoarthritis or any other more widespread joint disease.
Ideal patients for this method are young people with small isolated defects in the knee joint cartilage, preferably in the cartilage of femoral condyles.
These small, contained cartilage defects cause serious troubles to the young people but they are not osteoarthritis – they can, however, develop into osteoarthritis if untreated.
For more information one this method see www.carticel.com
Transplantation of a whole joint cartilage surface from amputated limbs.
In young patients with osteoarthritis limited only to one knee joint compartment, one may (at least theoretically) replace the worn out joint surfaces with new joint surfaces taken from amputated limbs.
As an alternative, one may place a new buffer – a new meniscus – between the worn out knee joint surfaces.
This is a theoretically sound idea:
- The cells of joint cartilage are used to starving – they receive their nourishment from joint fluid. Thus, they survive excellently the transplantation.
- The cells of joint cartilage are embedded in an avascular substance – cartilage matrix.
- Thus, they neither provoke rejection reaction in the host, nor will be influenced by such a reaction.
The advantages of this operation are:
- Less destruction of patient’s own skeleton, win time for a later total knee replacement
The disadvantages:
- Limited supply of knee joint tissues from amputated limbs, risk of blood transmitted infections, death and rejection of the transplanted tissues (in spite of theory)
- These transplantation operations are carried out at very few Centra around the world on strictly experimental basis.
Osteotomy
In a knee joint with only one joint compartment destructed by osteoarthritis, the mechanical axis goes no longer through the middle of the knee joint. Instead, the stresses concentrate on the already damaged compartment. Due to this concentration of stresses the cartilage damage continues and increases.
The surgeon may repair the distorted mechanical axis to the normal again. The operation is called osteotomy. Both knee joint bones may be operated on, but the most usual is the operation on the shinbone – tibia.
High tibia osteotomy
it is called high because it is is carried out high on the tibia, close to the knee joint.
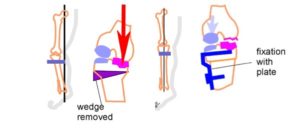
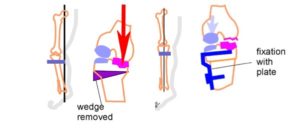
In this picture the inner (medial) compartment is damaged, the joint cartilage in the outer compartment is healthy.
A – The mechanical axis passes outside the knee joint, the knee is bent. The body weight (Red Arrow) passes through the already damaged medial compartment and damages it still more. The healthy outside part of the knee joint is not loaded.
The surgeon should change the limb axis so that the healthy outside of the knee joint will take the load.
The surgeon divides the tibia (the shinbone) below the knee joint (high) and takes out a wedge of bone on outside.
B – Then the surgeon pushes the lower part of the tibia to the outside. The divided bone ends come into contact and are stabilized in that corrected position by a plate and screw.
In this new position of the tibia, the body weight now passes through the healthy cartilage on the outside of the knee joint. (Blue Arrow)
The ideal candidates for this operation are young patients with damage in only one knee joint compartment and with a well-retained motion in their knees.
Advantages
- Lesser operation, does not open the knee joint, less risk for infection in the knee joint
Disadvantages
- Long rehabilitation with only partial weight bearing, risk of failed healing of the osteotomy and recurrence of the deformity
- Statistics show that about 65 – 75 % patients were still satisfied with the result of the tibial osteotomy ten years after the operation.
- The results of total knee replacement carried out after the high tibia osteotomy are not worse than the results in other patients. The operation is, however, more difficult and followed by higher rates of complications.
Arthrodesis – fusion of the knee joint
Nowadays, this operation is not an alternative for a total knee replacement. Instead, it may be the last operation after a failed total knee prosthesis.
In large statistics, arthrodesis of the knee joint was carried out in 0,0012% of patients with failed total knee replacement (Robertsson 1999).
After this operation the knee joint is gone and gone is also the pain. The knee joint is totally stiff.
References:
- Wai et al J Bone Joint Surg-Am 2002; 84-A.: 17-22
- Robertsson O et al Acta Orthop Scand 1999;70:467-72