Total knee operation – How is it done
Contents
- the anatomy of the knee joint
- patellofemoral joint
- mechanical axis of the knee joint
- range of motion
- stability of the total knee joint
- Total knee operation
- Computer assisted surgery
- lateral release of the patella
- Replacement of patella – an enigma
- Cemented and cementless fixation
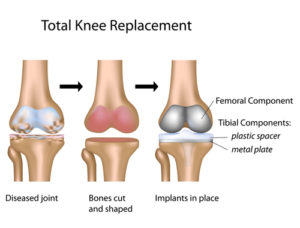
The name “Total Knee Replacement” is a misnomer.
In this operation, the surgeon removes only the damaged surfaces of the knee joint and then covers them with surface shells made of metal and polyethylene.
The proper name would thus be “the surface replacement of the knee joint”.
Here follows only a very short course on the principles of the operation itself.
If you wish to see more operation pictures already now, look at specialized websites
http://www.vesalius.com/graphics/archive/arch_gallery_list.asp
or ask your surgeon to loan a video showing the real operation procedure.
Anatomy of the healthy knee joint
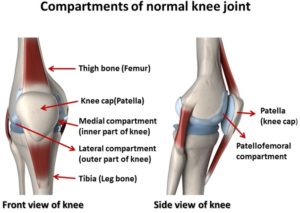
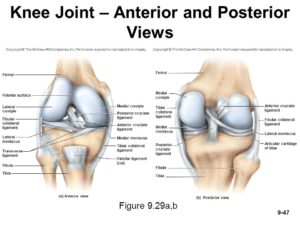
The knee joint is called a “prince” of joints. In it, two longest bones of the body, the thigh bone (femur) and the shinbone (tibia), articulate with each other. Moreover, a third bone, the kneecap (patella), articulates in the knee joint with the thighbone.
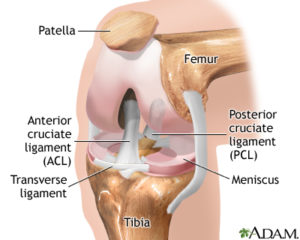
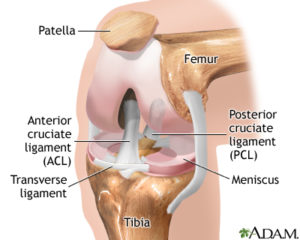
The picture presents a view on the bent right knee joint as seen when looking at it from the front, the kneecap (patella) was turned up.
The joint surfaces of the femur and tibia bones are called femoral and tibial condyles. The tibia (shinbone’s) condyles are flat, dish like, the femur (thighbone’s) condyles are round. The round femoral condyles thus articulate with flat tibial condyles.
Thus, the joint surfaces in the knee joint are not even congruent. To increase the congruence, Nature put two menisci (semilunar cartilages) between the incongruent joint surfaces of the femoral and tibial condyles (blue discs in the picture). As the knee joint moves, the menisci move too and increase the contact areas of the the joint surfaces.
The joint surfaces, condyles, are covered by a smooth, resilient joint cartilage. Joint cartilage has very low friction, in fact no man made bearing has as low friction and wear as healthy joints.
Stability
It is a wonder that such an incongruent joint is stable at all in all positions. The stability is, however, achieved by a clever system of ligaments, strong muscles, and by a strong but elastic joint capsule.
Two collateral ligaments (side ligaments) are placed on the sides of the knee, one on each side. These ligaments check the side stability of the knee joint.
Two cruciate ligaments (called so because they are “crossing” each other) are placed inside the joint in the space formed between the two femoral condyles. The direction of these ligaments is oblique to the long axis of the leg. These ligaments check the stability of the knee joint backwards and forwards, they restrain too much glide of the upper round (femoral) condyle on the flat lower (tibial) condyle.
One cruciate ligament is placed in front, the anterior cruciate ligament, the other one is placed behind it, the posterior cruciate ligament.
The strongest joint capsule is on the back side of the joint.
The strong muscle in the front of the knee joint is called quadriceps (Q) muscle, (not seen in this picture). Inside the tendon of the quadriceps muscle lies the kneecap (patella) and increases the muscle’s lever arm. The quadriceps (Q) muscle is always weakened in knee joint disease. Rehabilitation of this muscle to its former strength after total knee replacement constitutes a major part of postoperative gymnastic after this surgery.
The inner and outer halves of the knee joint make quite distinct joint spaces called compartments.
A) One space is on the inside (medial compartment), between the inner femoral condyle and the inner tibial condyle,
the other compartment is on the outside of the knee joint (lateral compartment) between the outer femoral an the outer tibial condyle.
Patellofemoral joint
B) There is a third compartment. This space is formed by the articulation of patella with the front surface of the femoral bone. As the knee joint bends and stretches, the patella glides in a track groove on the front side of the femoral bone. In English speaking literature the name of this compartment is patellofemoral, on European Continent the name is femoropatellar compartment.
This is a side-view that shows that patella articulates with the front side of the thigh bone. It is better seen on a cross section view. Today, the simplest way to produce cross-section view is to make a CT scan (Computer Tomography)
 On cross section (lower picture) of the knee joint one can see that patella conforms to a groove in the front side of the femoral condyle. In this symmetrical position the pressures on all parts of the patella’s joint surface are equally distributed and low. This symmetric position of the patella in the groove during the whole knee movement is thus important for the healthy function of the knee.
On cross section (lower picture) of the knee joint one can see that patella conforms to a groove in the front side of the femoral condyle. In this symmetrical position the pressures on all parts of the patella’s joint surface are equally distributed and low. This symmetric position of the patella in the groove during the whole knee movement is thus important for the healthy function of the knee.
The surgeon who replaces a knee joint must always secure the symmetrical position of the patella in the new knee joint.
Mechanical Axis Of The Knee Joint
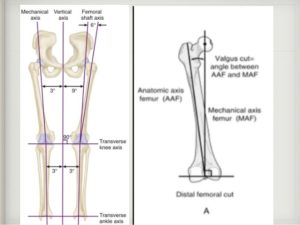
The mechanical axis of the knee is a line extending from the center of the hip joint to the middle of the ankle joint. This line is practically perpendicular to the ground.
In a healthy, well aligned knee joint, the mechanical axis passes through the middle of the knee.
(The anatomical axis is the axis extending along the shafts of the thigh and shinbone, not important in this context)
Only when the mechanical axis passes through the center of the knee joint, the stresses on the knee joint surfaces are uniform in all areas of the joint and well balanced.
In many knee joint diseases, the mechanical axis is disturbed and does not pass through the center of the joint. This disturbance results in the overload of distinct areas of the knee joint leading to their damage. The patella lies not symmetrically in its groove.
The surgeon must restore the mechanical axis of the knee joint during the total replacement surgery, i.e. he must put the new knee joint in such a position that the mechanical axis passes again through the middle of the new knee joint. The surgeon call it ” realigning of the total knee joint”. In this “realigned” position, the patella glides symmetrically in its groove. A total knee prosthesis put in badly aligned knee joint will be overloaded, the patella (or its prosthesis) will dislocate and eventually the whole total knee joint will loosen or break down.
You probably believe that this is an unnecessary complicated description of the anatomy of the knee joint. This picture is, however, very important for understanding the different kinds of total knee operations.
Some knee joint diseases engage only one compartment, most often the medial compartment of the knee. The surgeon then may replace only the surfaces of the engaged compartment, a much smaller operation.
The state of the knee ligaments is important for the result of a total knee operation. The better the function in the retained knee ligaments the easier is the total knee replacement operation and the better the chances for a good result.
The state of the ligaments in the knee joint decides, which kind of the total knee prosthesis the surgeon will use.
Although the natural joint cartilage is very resistant to wear, it may be destructed by
- disease (rheumatoid arthritis e.g.)
- trauma (damaged meniscus, fracture through the joint surface)
- load in wrong direction (knock or bow knee)
The most frequent cause of damage of the knee joint is, however, the so called idiopathic osteoarthritis. As the name idiopathic says, there is no known mechanism for this disease. It is often called degenerative joint disease.
Range of motion in the knee joint
Most people (even some orthopedic surgeons) see the knee joint as a simple hinge: In their view, the movement in the knee joint occurs in only one plane: the lower leg moves from the stretched position (extension) to the bent position (flexion).
In reality, the lower leg moves in the knee joint in all three planes: when it flexes (bends), it also rotates slightly and it swings to the side. And when the lower leg stretches (extends), it performs all these movements in the contrary directions.
This is a very important fact. A total knee joint constructed as a rigid hinge cannot resist the complicated forces generated in the knee joint during walking. Such hinge joint either breaks or the prosthesis loosen. In the past, this erroneous construction principle caused catastrophic failures of the hinged total knee joints.
All modern total knee prostheses imitate at least some of these complicated movements of the natural knee joint.
The range of motion in a healthy knee joint is from 0 degrees of extension to about 135 degrees of flexion. The possibility to extend the knee joint to 0 degrees (=straight line) is important, it guarantees the good function of the knee joint.
In everyday activities, the healthy knee joint seldom moves to more than 95 degrees of flexion.
Total knee joint seldom moves from 0 to more than 110 degrees of flexion only in well exercised patients. The range of motion in the total knee also depends on the type of the prosthesis.
Stability of the knee joint
The total knee joint must be stable if the patient should rely on it.
What confers stability to the total knee joint?
The commonly used total knee prosthesis consists in principle of two (or three, if patella is replaced) shells placed onto the destructed surfaces of the knee joint.
These shells have no intrinsic stability, they move freely in all directions against each other. It follows, that conventional total knee joint needs well functioning ligaments, muscles, and joint capsule for its stability.
Think of these ligaments, muscles, and joint capsule as an envelope or as a movable brace that keeps the total knee joint stable.
Also the patella is kept in place (in its symmetrical position) in the groove of the femoral condyle (lower end of the thighbone)
Once this envelope is defect or lacking and the knee joint is grossly unstable, the surgeon cannot use the conventional total knee prosthesis.
He must choose a total knee joint which has built in a clever mechanism that keeps the total knee stable. For more information see the chapter Linked total knee
The total knee replacement operation
The goals of a total knee replacement operation are
- the relief of pain
- the correction of knee joint deformity
- the restoration of knee joint motion
- the restoration of knee joint function
- creation of a stable knee joint.
Clear and simple. How the surgeon does it?
Disturbance of knee joint mechanics
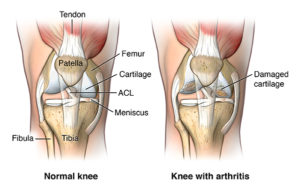
Note please, that the kneecap in this schematic picture was removed to allow better “insight” into the knee joint. The kneecap usually does not lies in place in worn out knee joints.
The knee joint to be replaced has not only damaged of joint cartilage, it is also distorted mechanically. The mechanical axis of the limb is distorted and does not pass through the middle of the knee joint. The ligaments are usually shrunken to keep the knee joint in the persistent wrong position. There are also contractures in the joint capsule keeping the knee joint in persistent bent position of the knee joint. (This is called contracture). Often there are only raw bone surfaces in contact.
Before the surgeon can put in the total knee prosthesis, he must not only remove the worn out joint surfaces surfaces, he must also correct the distorted position of the knee joint and restore the balance of the soft tissues.
All this the surgeon can achieve by making precise cuts through the bone ends so that when the prosthesis is put in place the mechanical axis of the knee joint will be restored, the ligaments will be tight, and the contractures will be corrected.
Making precise cuts
The surgeon opens the knee joint by a cut (incision) on the anterior site of the joint and inspects the damaged joint surfaces which should be removed.
The surgeon then removes all damaged knee joint surfaces with saws and drills much like those a carpenter uses.
The purpose is to provide close fit for the insertion of the components of a total knee prosthesis.
If it is deemed necessary, the surgeon resects the joint surface of the patella too. (Not shown in this picture)
Use of special tools for making precise cuts
Now, you must understand that during the operation, the patient legs are wrapped in thick surgical wraps, they look like a bulky packages, the pelvis and the hip joint are draped with sterile towels and hidden for the surgeon too. Not much precise orientation about knee axis on such a parcel.
In this situation, the precise cuts, necessary for balancing the tension in the knee’s ligaments and restoring the mechanical axis, must be made with help of special templates. The manufacturer provided the intricate tools to make these precise cuts at correct angles. Every total knee prosthesis model has its individual template. The surgeon and his staff must learn to use these tools with every model of a total knee prosthesis. That is why most surgeon are using only one or two total knee models.
In principle, these templates usually have two long rods, one reaching up to the hip joint area, one reaching down to the ankle joint. The rods join over the knee joint area in a cutting jig. This is in principle a plate with openings for sawblades of the cutting machine.
When the surgeon puts the sawblade in these openings, he knows that he makes the cutting of the bone ends in the right plane.
Before the operation, the surgeon marked, with help of X-rays, the center of the hip joint and pasted a bulging marker on the skin above it. He can palpate the bulging marker under the wraps. The surgeon puts the upper rod precisely above it.
The procedure is similar in placing the lower rod above the center of the ankle joint.
With the long rods in place, the opening in the cutting jig gives direction for the sawblade.
These templates are not exact instruments and the range of error in the cutting plane deviates up to 3 – 7 degrees from the ideal plane.
Computer assisted total knee surgery
To improve the precision of the total knee surgery, the surgeons and computer scientists are developing a computer assisted surgery of the total knee. This is a method under steady development, and the opinions about the usefulness of it are differing.
For more information about the method click here: Computer assisted total knee operation (link to another article)
Trial prosthesis to asses the precision of the cuts
After removing the destructed knee joint surfaces, the surgeon places a rectangular metal block (gray) between the cut joint surfaces to check the alignment. The block is equally thick as the future total knee prosthesis. With this block in place the surgeon will asses whether the cuts are appropriate to restore the mechanical axis of the knee joint.
In this picture the inserted block restores the mechanical axis of the knee joint and the ligaments are stretched appropriately.
If this assessment showed the right alignment of the mechanical axis of the new total knee, the surgeon then goes on to assess the function of the total knee prosthesis.
For this purpose, the surgeon places the trial knee joint prosthesis (gray) on the prepared bone ends and examines the range of motion and stability in the new knee joint.
Again, the trial prosthesis restores the mechanical axis of the knee joint and the ligaments are stretches appropriately.
In total knees where also patella was replaced, the surgeon controls the proper track of the patellar prosthesis during bending of the knee joint.
Putting definitive total knee prosthesis in place
If the range of motion is good, the stability of the joint is restored (the ligaments have proper tension) and the mechanical axis is restored, the definite prosthesis components are placed into position definitively.
The femoral (thigh bone) component of a knee prosthesis is a shell like plate, made from metal,
the tibial (shinbone) component of a knee prosthesis is a plate made of polyethylene (green), with small excavations for the engaging articular surface of the femoral component. Very often, the polyethylene plate is enclosed in a metallic envelope – metal backing – (blue), especially in cementless knee prostheses.
The surgeon pushes these components in place on the prepared bone surfaces and controls again the motion, stability and mechanical axis of the new knee joint.
Lateral release of the patella
If the surgeon replaces also the patella, that is a further step to do.
The surgeon places a trial patella prosthesis ( it looks like plastic button) in place and assesses the congruity between the femoral component and the patellar component during the whole range of movement.
When the congruity is good and the new patella glides stable in the groove of the femoral component, the surgeon places the definitive patellar component in place.
If the new patella does not glide in the middle of the groove of the femoral component, the bad tracking is often caused by tight ligaments pushing the new patella to the outer side of the total knee. The surgeon may cut these ligaments to enhance the stability of the new patella. This step is called “lateral release.”
Another reason for instability of the patellar component may be that the mechanical axis has not been corrected and still passes outside the total knee joint.
In this case the surgeon must correct the mechanical axis of the knee joint again, until the patella lies symmetrically.
If the patella is not replaced, the surgeon must still examine whether the patient’s own patella glides stable in the groove of the femoral component during the whole range of motion.
If the patella is not stable, it is often caused by tight ligaments pushing the patella to the outer side of the knee. The surgeon may cut these ligaments to enhance the stability (“lateral release”) as with the patellar prosthesis.
Then follows the suture of the operation wound. It is important, that after the wound suture there is no undue tension on the skin in the front of the knee during flexion of the joint.
Replacement of Patella (kneecap) – surgeon’s enigma
In the 1930’s, some orthopedic surgeons believed that patella ( the kneecap), like appendix, are unnecessary appendages of the body and may be removed at the surgeon’s discretion. Fortunately, this view did not prevail. The modern surgeons operating on a total knee joint are, however, facing a difficult decision: to replace or not to replace the patellar joint surface.
There are some good arguments why to replace always patella’s surface together with replacement of the other two knee compartments, but there are about as equally many good arguments against the routine replacement of the patellar joint surface.
You should discuss this question with your surgeon.
Patello-femoral osteoarthritis
There is also a special form of osteoarthrisis that damages only the joint between femur and patella (the so called patellofemoral joint). There are different causes of this isolated damage. In some patients it is caused by direct injury (in car accidents – dashboard injury), in other patients it is caused by bad position of the kneecap in the grove
This damage may cause severe pain and several surgical procedures were developed to treat this condition – all with varying success.
Some surgeons developed small joint prostheses that replace just these two joint surfaces: the patella’s surface and the frontal surface of the femoral condyle.
The success of these operations has been varying. At present, the surgeons are discussing whether this relatively small operation is justified.
The fixation of the total knee components to the skeleton
The surgeon may secure the components of the knee prosthesis in place with bone cement – cemented total knee joint or the surgeon may impact (hammer, blow) the components firmly onto the bone surfaces – press – fit fixation.
The components will be held there by the elasticity of the bone tissue – cementless total knee joint.
The advantages and disadvantages of cementless fixation of the total knee prosthesis are still discussed. Several reports demonstrated lately, however, that cementless tibial components have had higher rates of aseptic loosening.